I found advantages in giving hourly I.v boluses of Mg instead of infusion. 1 g hourly dose is given over 5 min. When we do that, we can maintain fluid input at desired rate, skip the Mg doses if urine output is unsatisfactory, and don't have to worry about inadvertent running of whole drip fast and overloading the patient with mg. the blood level fluctuation of mg is less compared to earlier 4 hourly im therapy, but may be more than iv infusion. anyhow, Considering the advantages and convenience, I recommend intermittant iv therapy
Friday, October 8, 2010
Magsulf intermittant I.v Therpy for Eclampsia
I found advantages in giving hourly I.v boluses of Mg instead of infusion. 1 g hourly dose is given over 5 min. When we do that, we can maintain fluid input at desired rate, skip the Mg doses if urine output is unsatisfactory, and don't have to worry about inadvertent running of whole drip fast and overloading the patient with mg. the blood level fluctuation of mg is less compared to earlier 4 hourly im therapy, but may be more than iv infusion. anyhow, Considering the advantages and convenience, I recommend intermittant iv therapy
Sunday, March 21, 2010
Cardiotocogram (CTG)
Variability and Reactivity: Variability is the result of fluctation of basal output of parasympathetic output from brain (Basal Ganglia), which is a sign of healthy brain. A depressed brain will have low intrensic activity (due to depressed reticular activating system). Reticular Activating System also controls sleep-awake cycle, so, it's depressed and we get reduced variability during fetal sleep also.
Reactivity is due to activation of fetal Sympathetic system during fetal movements. Sympathetic system is a crisis management system, and it accelerates the heart in anticipation of increased energy requirements. (not due to actual increased need, as reactivity occurs even with a small movement, which will not increase the oxygen demand in the fetus). During fetal Sleep, the motor system activity and activation of sympathetic system is low too, and as a result there will be no reactivity.
Deceleration: 3 types of decelerations :
Early Deceleration - is due to head compression in late labor, which creates a increased intracranial pressure, which increases fetal blood pressure by cushings reflex, which reduces the heart rates by means of nervous reflex from baroreceptors in Aorta. So, early deceleration indicates a healthy nervous system, and like variability and reactivity may be a sign of fetal well being, and it's absence is ominous.
Late Deceleration - is due to fetal hypoxia. When placental function is strained, during uterine contractions, there is a drop in fetal oxygen pressure, which depresses the fetal heart, and reduces the rate. Because fetus is yet unaffected during uterine relaxation, it forewarns the fetal hypoxia which is still occuring only during contractions, which may become more severe if contractions become harder and labor gets prolonged. Appropriate actions may be taken if labor is expected to take long time.
Variable Deceleration - is due to cord compression. variable deceleration can occur irrespective of presence or timing of uterine contractions. It can be distinguished by the shape of the curve, which is quite irregular and deep, and has two shoulders, which are initial and end accelerations. Initially, when cord is lightly compressed, the vein is occluded, which decreases fetal cardiac preload, causing fall in cardiac output, and there's mild tachycardia as a response (1st shoulder). Then the arteries are compressed, which increases the fetal blood pressure (compressing the fetal umbilical artery is like directly compressing it's aorta, as most of the flow from aorta goes to internal ileac, then to umbilical arteries), and causes reflex fetal bradycardia. The amount of bradycardia is proportional to fetal hypertension, which is proportional to umbilical compression, which is usually severe, abrupt, and irregular. At the end of compression, there's a phase, where arteries are released, but thinner veins are compressed, causing tachycardia.
Though any cord is liable for compresson, cords of IUGR babies, because they are thinner, than because of pausity of amniotic fluid, are more likely to be compressed. Though variable deceleration is not a direct result of fetal hypoxia, repeated compression, especially in a IUGR baby, can cause fetal hypoxia.
Case 1:
Early decelerations in Late labour. Patient delivered a healthy baby after one hour. (toco probes not kept properly, diagnosed as early by timing manually with patient's contractions)
case 2:
variable decelerations in early labor in a second gravida. delivered by CS, baby depressed, but recovered well.
Thursday, March 18, 2010
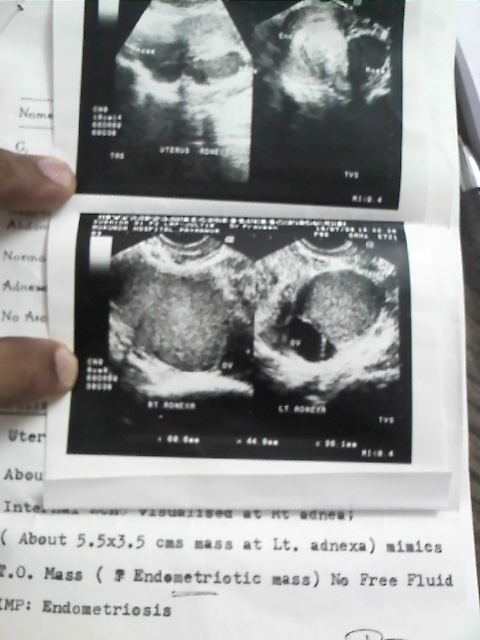
Depot Provera in endometriosis
Medical Treatment for endometriosis can be tried in unmarried girls, those who have finished family, and in whom pain is the troublesome symptom. Two strategies for medical treatment are:
- pseudo-menopausal regime
- pseudo-pregnancy regime
Pseudo- menopausal state is achieved using GnRH analogues, and pseudo-pregnancy regime by progestrone. both alters the hormonay mileu, suppresses HPO axis (there by reduces the growth of ectopic endometrium), alters peritoneal immune system (controlled by hormones and is associated with the development of endometriosis).
Pseudomenopausal regime is associated with menopausal symptoms, osteoporosis, and GnRHa s are costly. pseudo-pregnancy regime can be administered much more easily, using Depot Provera (Medroxy Progestrone Acetate). It's given once in 3 months injection (more frequent injections as adviced in certain texts are not required). It maintains a constant level of progestrone in the body, suppresses HPO, and keeps endometrium thin. We expect the ectopic endometrium also to be maintained thin, and together with altered immune function, endometrium is expected to heal.
Unpredictable irregular bleeding is the side effect with Depot Provera. As endometrium is thin, estrogen can be administered, which heals the endometrium. (Ethnyl Estradiol 10mcg TDS during bleeding days). Patient is adviced to take estrogen during bleeding days. Initially during therapy bleeding is more frequent. It's usually minimal or scanty, not painful. gradually, bleeding becomes quite infrequent, even amenorrhea will occur. There's no fear of permanant amenorrhea, as the state is purely hormonal, and any time, on treatment with estrogen-progestrone, normal cycles can be brought about.
I have treated many cases of endometriosis with this regime. Symptomatic relief is great, and ultrsonically regression of endometriosis can be proven. There's little side effects or discontinuation of treatment. Patients are so happy that, they refuse to stop the drug.
Here's one of the patients, who was P2L2, had troublesome secondary dysmenorrhea (Secondary dysmenorrhea to be distinguished from Primary Dysmenorrhea, which is sever on the first day, and is alleviated as the bleeding increases on the second day. Secondary dysmenorrhea becomes more severe as bleeding increases on second and third day.) She was given Depot Provera 2 years back. She took 2 injections (6 months) and as the symptoms reduced, she stopped the drug, and was having normal cycles. She came back again recently, as her symptoms have reappeared. I sent her for scan expecting to see the lesions increased. To my surprise, the lesions had reduced drastically (even with no treatment for 2 years). This not only proves the effect of Depot Provera, but also that endometriosis can spontaneously regress.
2 years back:
Now
Wednesday, March 3, 2010
Cervical encirclage
Cervical circlage is very much misused surgery. The use of circlage is often questionable. And in cases where circlage seems to have worked, we have to doubt, if it would have gone well, even without cirlage also.
case:
This is a second gravida, first term cesarean, who had short cervix and membranes bulging into cervix in her routine second trimester scan. As her first pregnancy was normal, I told her to continue her pregnancy her normal, without even advising her rest. She has gone to term, and is posted for elective CS today!
Saturday, February 20, 2010
Rationalising Hormonal treatment for DUB (Dysfunctional Uterine Bleeding)
HPO axis - a digital system : HPO axis is an independent functional unit, that's anatomically distributed at distant sites in the body. It has an amazing behaviour that's either it's normal, when it's ovulatory, secretes estrogen and progesterone in a regular oscillatory pattern. Or, it's abnormal, when it's anovulatory, and hormonal secretion is almost continous and in constant quantities (only estrogen, no progestrone). This is so, because it's the natures check against impregnation at unwanted times. Nature takes care that, the organism doesnt become pregnant, at unoptimal time, during it's physical and enviornmental crisis, and endanger it's pregnancy and itself. Nature does this by checking the ovulation. so, it's interesting that, all the system in the body, the psyche, hormones, physical status, nutrion etc effect HPO, though it is not effected by the end organ -uterus itself. Thus HPO is aware of the health status of the body itself, but unaware of the bleeding problems in the uterus. Probably, in the wild, it needn't know because, a woman had hardly any time for menstruation. The ovulation acts as a check valve. If the condition are suboptimal, the nautre aborts the sytem, before ovulation, and prevents a pregnancy.
In a Normal Ovulatory cycle, after the endometrium is shed, it's healed by the estrogen coming in in the following cycle. Estrogen proliferates the endometrium rapidly and heals it. Thus, if we take the lesson from nature, estrogen is the best to stop a bleeding. Progestrone in the secretary phase makes the endometrium compact, and also, at it's withdrawal causes, sever vasospasm, which causes global shedding of the endometrium, and also, limits the bleeding. Thus, the bleeding mechanism, has a natural builtin mechanism to prevent excess bleeing too. This, when the system is ovulatory.
In anovulatory state (not cycle, as HPO has stopped oscillating) the HPO gives out continous estrogen, which proliferates the endometrium beyond the capacity of it's stroma, endometrium is shed from places, thus last longer, and because there's no vasospasm due to absence of progestrone, bleeding is heavy.
Thus in treating DUB, our aim will be to:
- 1. make sure, the uterus is sequentioally stimulated by estrogen and progestrone
- 2. to convert anovulator HPO into ovulatory (if possible)
In an anovulatory woman, we can acheive our first goal, by supplementing progestrone. She gets estrogen which comes at a steady state from the HPO, so, we have to leave about 2 weeks after the menstruation, then give her progestrone tablets for about 10 days.
If the patient presents with bleeding, we have to arrest bleeding. The patient cant accept to wait till bleeding stops naturally. We have to give her estrogen to acheive this, then continue estrogen for about 2 weeks, followed by progestrone. An anovulatory woman will have slightly reduced estrogen, than the end-follicular phase of a ovulatory woman. (if the estrogen increases to normal level, she'll have LH surge and ovulation. Thus ovulation acts as a check against hyper-estrogenemia) Common practice is to give such women progestrone at higher dose, but usually she bleeds irregularly on such treatment. Estrogen acheives hemostases effortlessly.
To make the HPO ovulatory, it's better to suppress it completely, for sometime, and then, when it starts functioning again, probably, it'll be ovulatory. OC pills (estrogen+progesterone) is best to acheive this. HPO is complex system, with many interacting hormones. We cant convert it to ovulatory, by trying to make small changes. The tendency to anovulation varies among women, thus, some women have strong tendency to anovulation, owing to their enzyme variations, fat levels,other hormone levels etc. Once a woman becomes anovulatory, the HPO remains in that state, unless it's put back into track by some luck. So, if a woman bleeds irregulary 3 times in 8 months, she didnt have 3 anovulatory cycles, rather, she was anovulatary for 8 months, since, the HPO became deranged in the first instance.